- May 9, 2024
Understanding the Underpinnings of Sensory Hypersensitivity in Autism
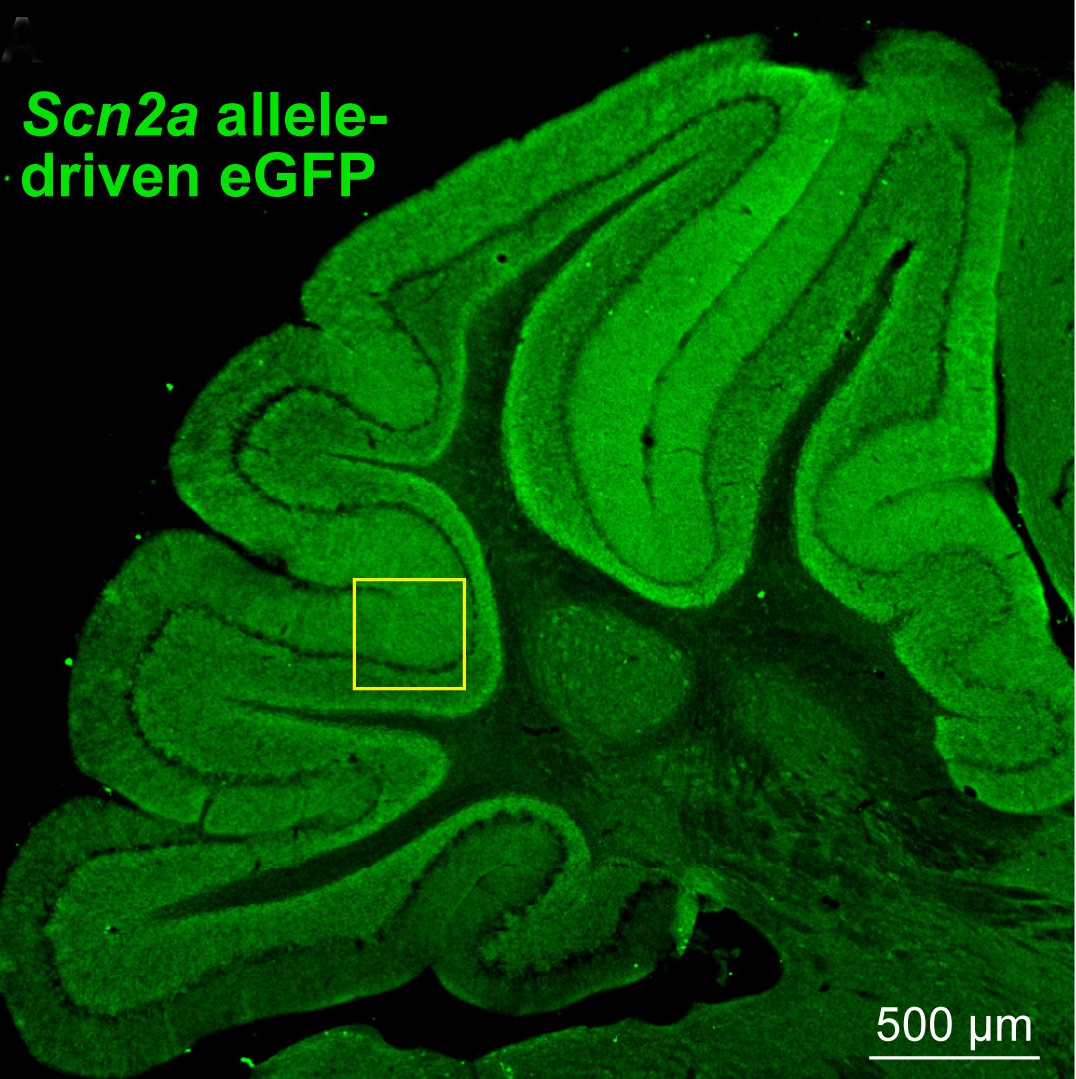 A section of mouse cerebellum. Credit: Wang et. al., 2024, Neuron.
A section of mouse cerebellum. Credit: Wang et. al., 2024, Neuron.
People who experience sensory hypersensitivity have a heightened awareness of and reactivity to sensory stimuli, such as sound, sight, touch, and taste. Sensory hypersensitivity is a symptom often associated with autism spectrum disorder (ASD), as more than 90% of children who have ASD experience this sensory challenge.
Researchers examining the neural underpinnings of sensory hypersensitivity have often focused on the role of the forebrain—an area in the front of the brain involved in processing sensory stimuli and regulating behaviors and emotions. However, new research suggests that brain circuitry that supports sensory reflexes—which occur at a much earlier stage of sensory processing—could also be contributing to this sensitivity.
What did the researchers do?
To learn more about the neural underpinnings of sensory hypersensitivity, a new NIMH-funded study by Chenyu Wang, Ph.D., a researcher at the University of California, San Francisco, and colleagues looked at brain areas that control the vestibulo-ocular reflex. This reflex stabilizes images on our retina by causing our eyes to move in the opposite direction of our head.
The researchers examined how the brain controls this reflex in people and mice with a genetic mutation called SCN2A loss of function. SCN2A loss of function has the strongest association with ASD of any known genetic mutation. The SCN2A mutation impacts the way neurons move charged particles, called ions, into and out of the cell. This, in turn, affects the way cells (including those involved with the vestibulo-ocular reflex) electrically communicate with each other.
Participants included children between the ages of 3 and 10 with the SCN2A loss of function genetic mutation diagnosed with ASD, as well as similarly aged children who did not have the mutation or were diagnosed with ASD. All participants wore lightweight helmets that tracked both their eye and head movements. The researchers found that the vestibulo-ocular reflex was hypersensitive in children with the SCN2A loss of function genetic mutation compared to those without the mutation. The researchers found that mice with the Scn2a loss of function mutation also showed this pattern of heightened vestibulo-ocular reflex behavior.
To find out what might be causing this pattern of vestibulo-ocular reflex behavior, the researchers recorded electrical activity in the brains of mice with the Scn2a loss of function mutation. They found that the activity between cells involved in supporting the vestibulo-ocular reflex (called Purkinje and cerebellar granule cells) did not change in response to differing levels of head speed and movement, unlike what would be seen in mice without this genetic mutation. This lack of cell activity adaptation was found to be driven by the Scn2a loss of function mutation in the granule cells.
To see if a typical vestibulo-ocular reflex could be restored, the researchers administered a gene-based therapeutic to mice that targeted the Sn2a loss of function mutation when they were either 3 days old or 30 days old. The researchers were able to fully restore typical vestibulo-ocular reflex behavior in mice treated at 3 days old, but restoration was only partial in mice treated at 30 days old, suggesting there is an early developmental period that cements aspects of this reflex.
What do the results mean?
This study shines light on the neural processes involved in a specific symptom associated with ASD—sensitivity to sensory stimuli. In addition, since the vestibulo-ocular reflex was hyperactive in children with SCN2A loss of function-associated autism, the findings suggest an eye reflex test could be used in the future as an early identifier of ASD. Additionally, a gene-based therapeutic restored typical vestibulo-ocular reflex behavior when given to very young mice with Scn2a loss of function, suggesting a possible way to ameliorate sensorimotor dysfunction in the future. The study also suggests that cerebellum-dependent reflexes, like the vestibulo-ocular reflex, may prove to be generalizable and translatable markers for determining the effectiveness of potential therapies that aim to address sensorimotor symptoms commonly experienced by people with ASD.

